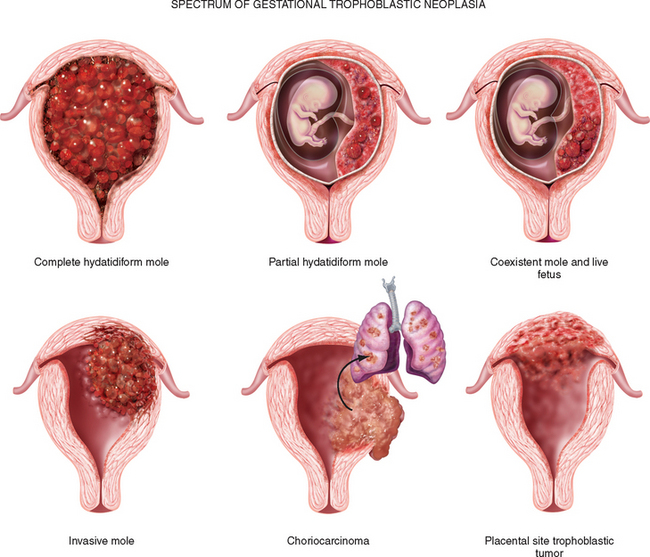
Gestational trophoblastic disease (GTD) is a group of rare tumors that involve abnormal growth of cells inside a woman’s uterus. GTD does not develop from cells of the uterus like cervical cancer or endometrial (uterine lining) cancer do. Instead, these tumors start in the cells that would normally develop into the placenta during pregnancy. (The term gestationalrefers to pregnancy.)
Types of gestational trophoblastic disease
- Hydatidiform mole (complete or partial)
- Invasive mole
- Choriocarcinoma
- Placental-site trophoblastic tumor
- Epithelioid trophoblastic tumor
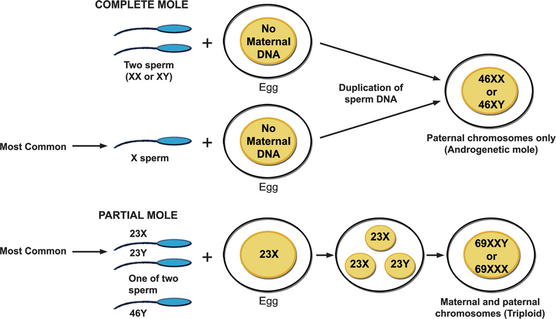
Normally, at fertilization, a single egg with 23 chromosomes fuses with a single sperm with 23 chromosomes, resulting in a new organism with 46 chromosomes. This can go wrong in two ways, so we have two kinds of moles – complete, or classic, and incomplete, or partial mole. Both lead to an abnormal proliferation of placental cells, and an abnormal placenta.
Complete mole appears when a chromosomally empty egg fuses with a normal sperm, and the sperm genetic material duplicates to form a 46 chromosome organism. However, this organism doesn’t have both maternal and paternal chromosomes, so the mole develops into a mass rather than developing into a fetus.
With a complete mole, the placenta secretes a huge amount of HCG. So affected females present with signs of pregnancy, like missed periods, and a positive urine pregnancy test.
Incomplete mole, on the other hand, appears when a normal egg is fertilized by two sperm – which forms an organism with 69 chromosomes, that usually develops into non-viable fetal parts.
Invasive mole (formerly known as chorioadenoma destruens) is a hydatidiform mole that has grown into the muscle layer of the uterus. Invasive moles can develop from either complete or partial moles, but complete moles become invasive much more often than do partial moles. Invasive moles develop in less than 1 out of 5 women who have had a complete mole removed. The risk of developing an invasive mole in these women increases if:
- There is a long time (more than 4 months) between their last menstrual period and treatment.
- The uterus has become very large.
- The woman is older than 40 years.
- The woman has had gestational trophoblastic disease in the past.
Choriocarcinoma is a malignant form of gestational trophoblastic disease (GTD). It is much more likely than other types of GTD to grow quickly and spread to organs away from the uterus.
Placental-site trophoblastic tumor (PSTT) is a very rare form of GTDthat develops where the placenta attaches to the lining of the uterus. This tumor most often develops after a normal pregnancy or abortion, but it may also develop after a complete or partial mole is removed.
Most PSTTs do not spread to other sites in the body. But these tumors have a tendency to grow into (invade) the muscle layer of the uterus.
Most forms of GTD are very sensitive to chemotherapy drugs, but PSTTs are not. Instead, they are treated with surgery, to completely remove disease.
Signs and symptoms
- irregular vaginal bleeding range from light spotting to heavy bleeding, and parts of the mole may even be eliminated, and they look like grapes, or cherry-like clusters.
- hyperemesis (due to huge amount of HCG)
- excessive uterine enlargement
- early failed pregnancy.
- urine pregnancy test in women presenting with such symptoms.
- physical examination shows a uterus that’s too big for gestational age since the mole grows much faster than a normal pregnancy would.
Rarer presentations in complete hydatidiform (high HCG level) include hyperthyroidism, early onset pre-eclampsia or abdominal distension due to theca lutein cysts. HCG has a subunit that’s similar to TSH, FSH, and LH. This causes symptoms of hyperthyroidism – like insomnia, anxiety, tachycardia, and palpitations, as well as the formation of theca lutein cysts on the ovaries, which can cause adnexal mass symptoms like pain or pressure on the affected side.
Very rarely, women can present with acute respiratory failure or
neurological symptoms such as seizures; these are likely to be due to metastatic disease.
Diagnosis
- ultrasound diagnosis of a partial molar pregnancy is more complex; the finding of multiple soft markers, including both cystic spaces in the placenta and a ratio of transverse to anterioposterior dimension of the gestation sac of greater than 1.5, is required for the reliable diagnosis of a partial molar pregnancy.
- Estimation of hCG levels may be of value in diagnosing molar pregnancies: hCG levels greater than two multiples of the median may help.


